Do I Have a Stress Fracture Quiz
do i have a stress facture quiz
March fractures (metatarsal stress fractures) are bone fractures of the midfoot and a subgroup of the so-called stress fractures or fatigue fractures. In this case, recurrent stress below the fracture threshold results in micro-fracturing within the bone and subsequently in a bone fracture. The clinical picture was first described in the second half of the 19th century by the Prussian military physician Breithaupt in young recruits after prolonged marching. Even today, marching fractures are frequently diagnosed in young untrained soldiers after marches.
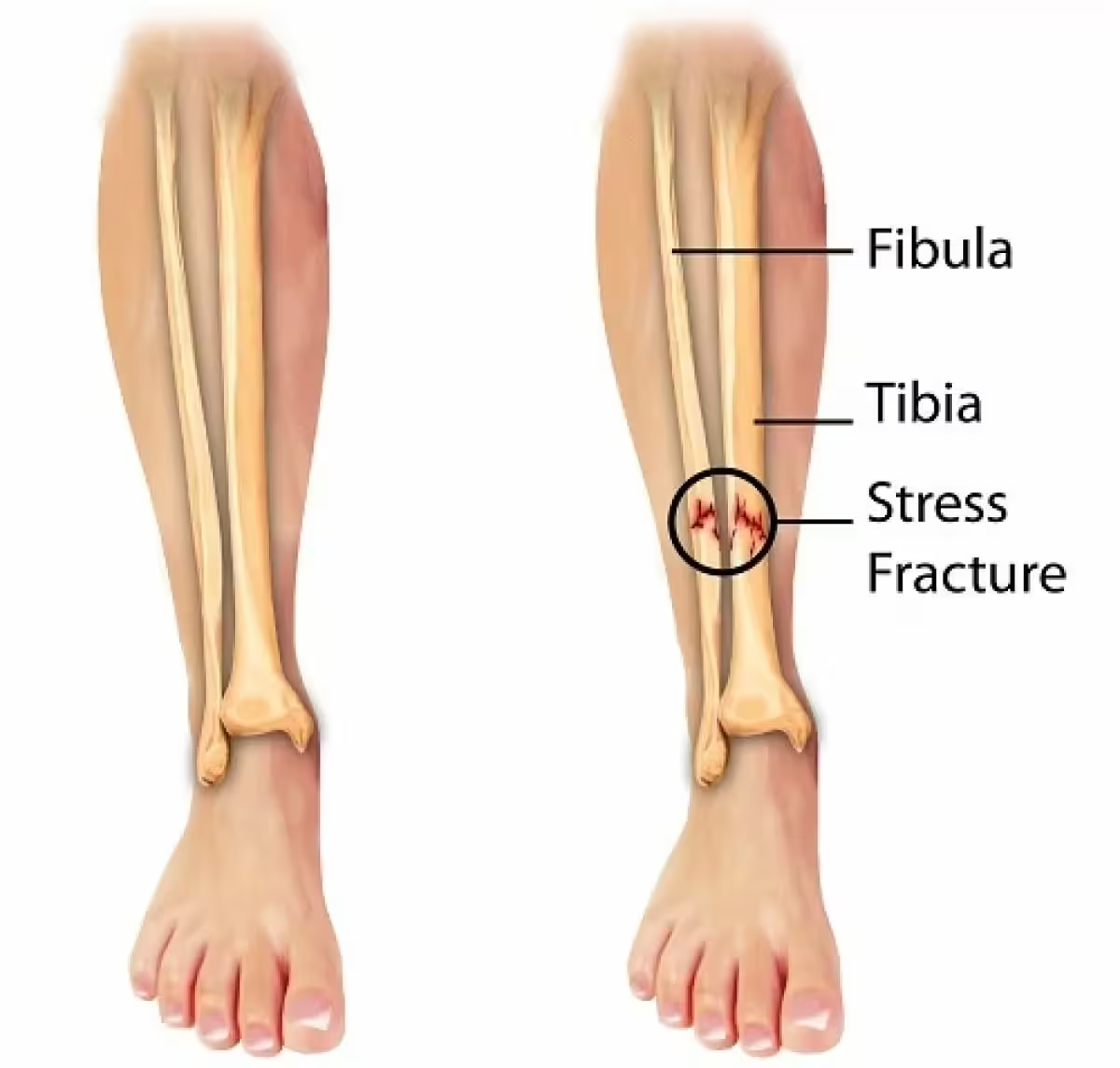
The human bone is constantly remodeling; thanks to bone metabolism, its structures can adapt to the respective requirements. In stress fractures, recurrent loads below the fracture threshold cause micro-fracturing within the bone bellows (small bars of bone tissue that make up the spongy interior of the bones), with insufficient repair processes resulting in stress reactions and fractures. As expected, the stressed lower extremities are particularly affected, especially the foot skeleton, the tibia, the fibula, and the neck of the femur.
These are primarily sports injuries, especially in track and field, running, and soccer. More extensive studies assume that up to ten percent of all sports injuries involve stress fractures.
Causes
The exact causes of stress fractures are not yet clearly understood. However, some risk factors favor the occurrence and thus provide clues to the development of stress fractures. These are primarily:
Eating disorders: Larger studies have demonstrated that stress fractures are more common in overeating and undereating, such as in some disciplines among competitive anorectic athletes.
Women are more often affected than men: hormonal imbalances are an additional risk. In young women with menstrual disorders and women in menopause, these injuries are clustered. Estrogen deficiency leads to decreased bone density and, thus, more fractures. Long-term cortisone therapy also does the same thing.
Mechanical factors such as axial and foot misalignments also increase the risk of such injuries.
Symptoms and Course
The complaints occur after prolonged, unaccustomed exertion or after a change in training and an increase in activity, for example, before competitions.
In typical marching fractures, patients complain of pain in the forefoot and midfoot, which increases with exertion. The metatarsus has pressure pain swelling, especially over the affected section. Usually, the second and third metatarsal bones are affected.
Diagnosis
The suspected diagnosis results from the medical history and the clinical findings. The classic X-ray examination often shows no indications in the acute stage, leading to misinterpretations. Only after at least 14 days are zones of bone resorption and a possible beginning formation of new bone tissue after the fracture (callus formation) recognizable in the X-ray image.
MRI examination is the method of choice today if there is any suspicion. Here, changes are already detected in the early stages, which supports the diagnosis. A distinction is made between different stages. Initially, fluid accumulation in the bone (bone edema) with a clear swelling in the fracture area. Later, a fracture line with reparative processes can be detected.
Scintigraphy shows an apparent increase in activity even in the early phase, which can help to establish the diagnosis if the X-ray is unclear.
The CT scan is only helpful for specific questions, for example, when surgery planning is rarely necessary.
Therapy
March fractures in the metatarsal region are usually not displaced and can thus be treated conservatively. Only rarely does secondary displacement of the fragments occur, which then requires surgical treatment. This is also true for most other stress fractures. Only a few fractures are at risk of slipping and therefore require surgical treatment. This applies, among others, to fatigue fractures in the area of the femoral neck and the lower leg. In this case, the general rules of osteosynthesis in operative fracture treatment apply.
Conservative treatment depends on the stage of the disease and the patient’s complaints. It consists primarily of the relief of the affected skeletal section. In some cases, a four to six-week ban on sports is already sufficient, whereby even suitable sporting activities such as swimming and cycling may be permitted without symptoms. In the initial phase and cases of severe pain, relief on forearm crutches may also be appropriate. Complete immobilization in a plaster cast or adapted braces are rarely necessary. For the actual marching fractures, customized insoles with a firm sole and support of the metatarsal arch are helpful.
Supportive medication is used primarily by administering analgesics for pain relief. Medicines from the group of NSAIDs (non-steroidal anti-inflammatory drugs) are mainly used, which also combat the sometimes considerable swelling and accompanying edema due to their simultaneous anti-inflammatory effect. Vitamin D and calcium are thought to stimulate bone metabolism and are often prescribed as supplements. The administration of calcitonin and bisphosphonates is also occasionally reported, but evidence of their efficacy has yet to be provided.
Physical measures such as cold application and electrotherapy may be helpful for symptom relief.
There are reports from competitive sports of good results using ESWT (extracorporeal shock wave therapy) to accelerate bone healing. This effect has been proven in the treatment of pseudarthrosis.
It is also necessary to analyze and treat risk factors such as malnutrition and hormone deficiency.
Conclusion
March fractures are a unique form of stress fractures in the metatarsal region. Young soldiers and athletes in running sports are mainly affected. If diagnosed early, it is usually treated conservatively. The long-term prognosis in terms of resilience and sports ability is good.
Disclaimer
Please note that this quiz is for informational purposes only and is not a substitute for medical advice. If you are experiencing pain or discomfort, please consult with a qualified medical practitioner for proper evaluation and diagnosis. Stress fractures can be diagnosed through imaging tests, such as X-rays or MRI scans. Early detection and treatment of stress fractures can help prevent more serious injuries and long-term complications.